There was an understandable healthy degree of scepticism at last week’s Digital Healthcare Show at London’s Excel centre – an issue recognised by the new Chief Executive Officer of NHS Digital (NHSX) Matthew Gould.
In his keynote presentation, Gould acknowledged that NHSX follows a long line of much heralded IT change across the health system, such as Care Dot data and the National IT programme.
“I know you’ve seen this movie before, the big bang announcement with a shiny new leader who has all the optimism before the fall. I understand the level of scepticism that we are going to be operating in.”
But he explained that NHSX will bring departments together: The Department of Health and Social Care for national policy matters, NHS England for links to the system and NHS Improvement for spending controls.
Careful about over-promising, Gould said NHSX will focus on overseeing digital transformation, focusing on issues such as standards “The most important thing we will do is set the rules so our systems can talk to each other, so that our systems are secure and help keep patient data safe.”
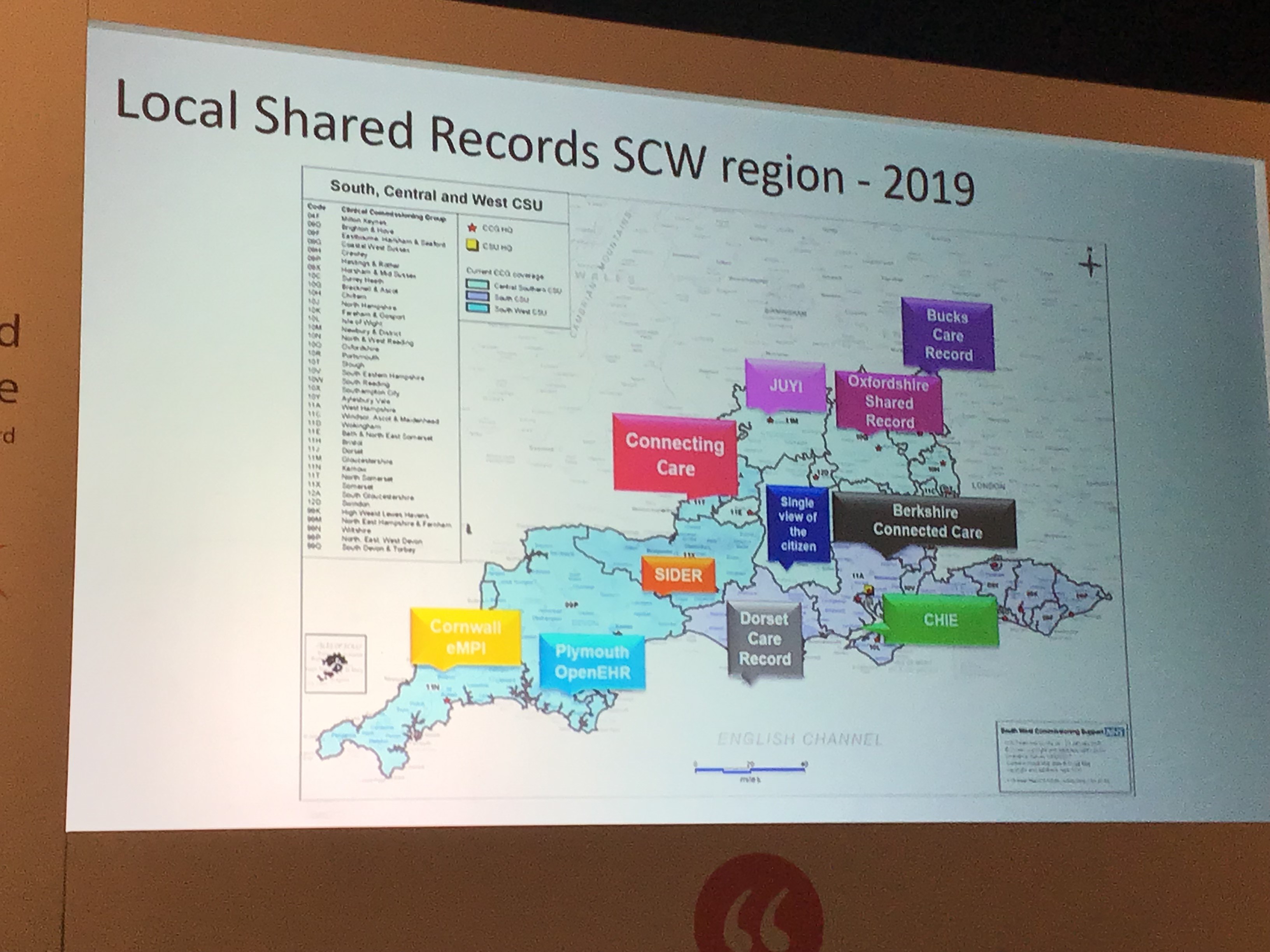
 This was highlighted by Bristol’s Connecting Care head of engagement Fran Draper, who talked about the past six years of partner and patient interaction. Draper said the key to their success had been making interoperability work, having visionary people at the top, real drive among the Executive, being bold, and at times, making a leap of faith. It had been a long journey but one with plenty of rewards along the way.
This was highlighted by Bristol’s Connecting Care head of engagement Fran Draper, who talked about the past six years of partner and patient interaction. Draper said the key to their success had been making interoperability work, having visionary people at the top, real drive among the Executive, being bold, and at times, making a leap of faith. It had been a long journey but one with plenty of rewards along the way.
Working closely with their local HealthWatch, having a good public facing website and even better staff intranet has helped and Connecting Care now has 20 systems sharing data and 24 organisations viewing.
With hospitals, adult and children’s social; care, mental health, community health, radiology, controlled medications, GP records, out of hours, NHS Spine, demographics and organisational data on board, Connecting Care has had 550,000 records viewed over the past two years, with an average of 37,000 a month and rising.
Quality data is key and this was highlighted by Dr Justin Whatling, from the Faculty of Clinical Informatics, who talked about population health management opportunities. Whatling said population health was all about the need to improve patient experience, the health of the population, improve staff experience and reduce the cost of healthcare.
While there is plenty of ongoing analytics work, it is now well directed for health and social care, and Whatling said this was a key role for the Local Health and Care Records (LHCR’s). However, data is only as good as the data system in place and Lewisham found a number of problems when looking to use data to diagnose diabetes. Issues with uncoded patients and lack of accurate data meant some patients needed to be specifically validated by their GP.
 Mike Trenell, Director of NIHR Innovation Observatory, said there was still not enough information about people’s lifestyles and behaviours: “Scientists are great at sequencing genomes but we need to embrace the complexity of disease and behaviours, the environment and people’s well-being. Medics need to get to know their postcodes.” He added that too much treatment is done on a silo basis, not taking in the wider picture and normative behaviour.
Mike Trenell, Director of NIHR Innovation Observatory, said there was still not enough information about people’s lifestyles and behaviours: “Scientists are great at sequencing genomes but we need to embrace the complexity of disease and behaviours, the environment and people’s well-being. Medics need to get to know their postcodes.” He added that too much treatment is done on a silo basis, not taking in the wider picture and normative behaviour.
Perhaps the overriding message coming out of the conference was, for all the digital transformation taking place, the need to put people first is paramount.


