Delegates attending Orion Health’s annual conference in Manchester this week were given updates on precision driven health, medicines management, business intelligence and population health tools and heard about some of the latest regional information sharing.
Orion Health works across the world at 58 Health Information Exchange sites from 22 offices in 15 countries with 110m+ patient records. So, it was interesting to hear from Orion country leads about digital health work taking place as far afield as the United Arab Emirates, the United States, Canada, France, Spain and Australasia.
Closer to home, the company welcomed our Hampshire neighbours CHIE to their first conference. And it highlighted its work with Boots, where it is now live in 350 stores since proof of concept in 2015. OH technology currently provides platform and forms-based technology to support Boots initiatives such as influenza and hair retention.
Chief executive Ian McCrae showcased the company’s enthusiasm for all things precision medicine and machine learning and how the business can harness data from the determinants of health to improve care and efficiency.
Machine learning algorithms, with its benefits of having clear and measurable statistics, cropped up throughout the day. OH’s research director Kevin Ross said delivering this into clinical workflow was currently one of the largest gaps in healthcare today. Ross talked about some of Orion’s latest products including its Machine Learning Manager, Document Tagger and Data de-identifier.
The company, which employs 750 people, has seen changes over the past 12 months, delisting from the New Zealand and Australian stock exchanges and completing a share buy-back in March. McCrae said Orion had “created a whole bunch of start-ups” and “we are really starting to see innovation coming through that.”
Focusing on lines of business has also enabled the company to set up development centres in more regions, “closer to our customers. Having developers working with clinicians” means faster innovation and testing.
There were some great customer presentations. Jim Doherty, NHS Highland clinical director ehealth, speak about how it was possible to create a single view of patient data across the remote Highlands and Islands of north and west Scotland, as well as touching on the benefits being realised and future plans. Overcoming collaboration issues involved with 14 health boards and numerous local authorities, Doherty is looing forward to social work and GP data, care pathways, collaborative worklists and cloud hosting coming on stream in the next phase.
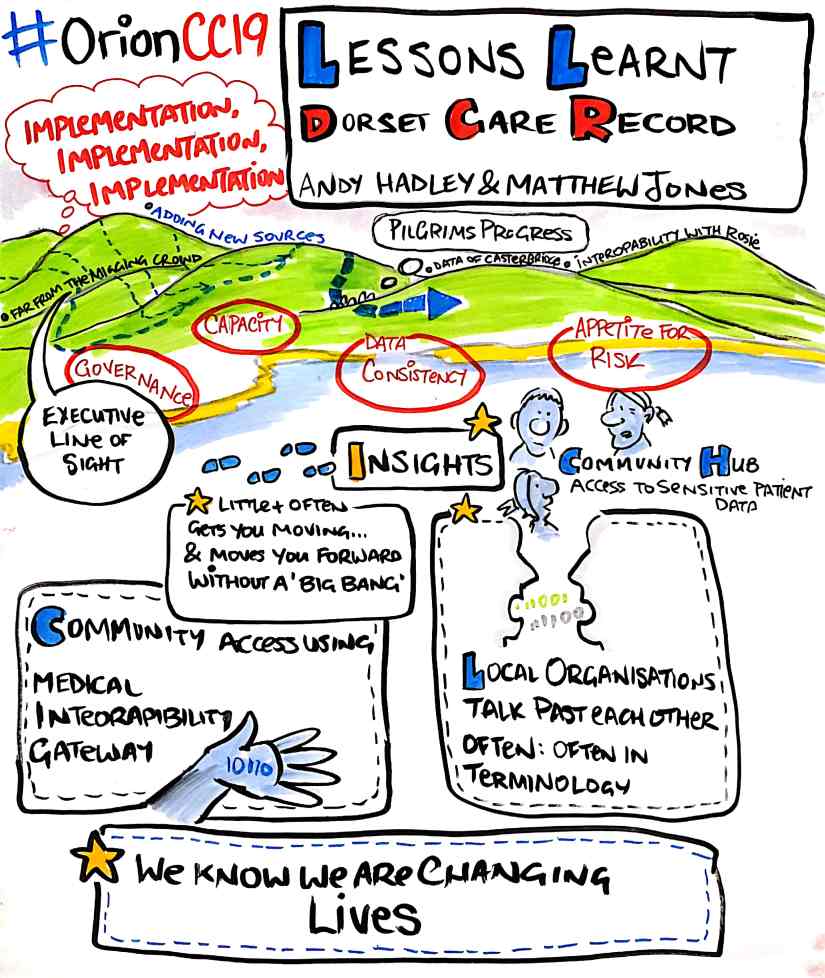
The first double-act of the day fell to our technical architect Andy Hadley and Channel 3 consultant Matt Jones, who talked about the key challenges, successes and future plans of the Dorset Care Record. Highlighting the challenges, Jones grouped them into four areas – governance, capacity, data consistency and risk appetite – issues that seemed pertinent to other customers in the room.
Future plans include bringing social care into the record to ensure there is comprehensive demographic data across health and social care; additional data entering DCR through documents, Admissions, Discharge and Transfer’s and departmental feeds. Single sign on will help practitioners access directly into the relevant record from source systems, while our initial focus on the maternity care pathway will hopefully lead to many future use cases and the holy grail of a citizen’s portal personal health record.
Hadley talked about the ongoing discussions with Orio and Wellsky (formerly JAC) over the key components of a One Medication Record – an issue that is being taken forward by Wessex Care Records.
Stephen Beattie, e-health programme manager for the Business Services Organisation in Northern Ireland, talked about the phases of its “My Care Record” patient portal for those living with dementia as part of the Northern Ireland Electronic Care Record (NIECR).
Phase one, which went live in January included hospital appointments, the creation of a health library, shared files, including video, PDF and word documents, and the introduction of a circle of care. Due to likely interaction between patients and staff a disclaimer was provided to stressed that the system should not be used for urgent health queries. This is currently being followed by a second phase which included goals, clinical documents and community appointments.
Among the lessons learned was the surprise to the team that appointments were the most viewed screen during the pilot; the delight that the health library is proving useful for patients with a new diagnosis and the fact that identifying patients who want to use the system has been more problematic than expected. The Circle of Care was not extensively used by the clinical team during the pilot so plans are in place to auto populate teams and organisation details for phase two.
The final phase, due next year, will include medications, lab results and enhancements following pilot feedback. Lab results will be interesting as there is an ongoing debate with clinicians about how it is presented and what exactly is a normal range.
So which pathways are next on the list for the award-winning NIECR team? Beattie says it’s exciting to be in a situation where people are coming up with asks – whether it be diabetes, neurology, respiratory care, heart failure, obstetrics, ophthalmology, mental health or orthopaedics….
Ends


